For US Healthcare Professionals Only
Managing Adverse Reactions
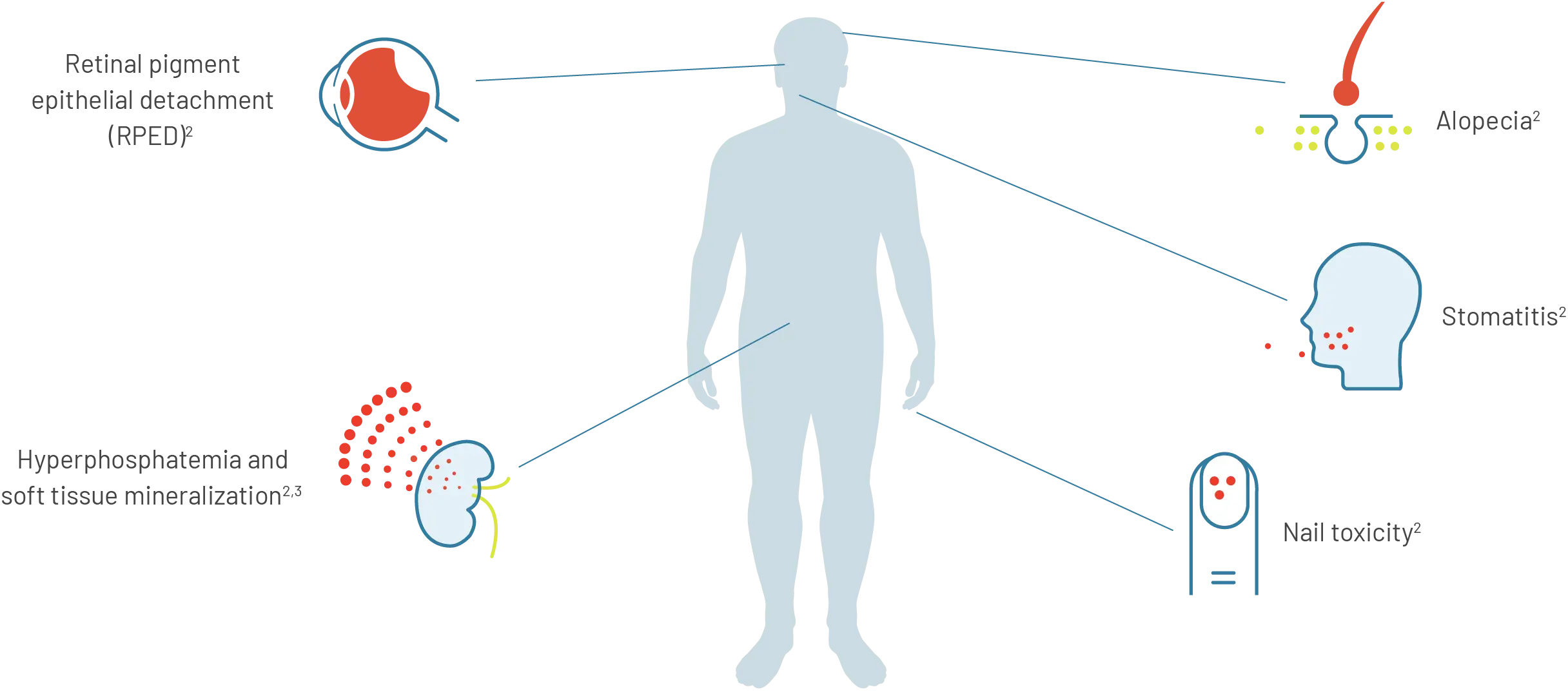
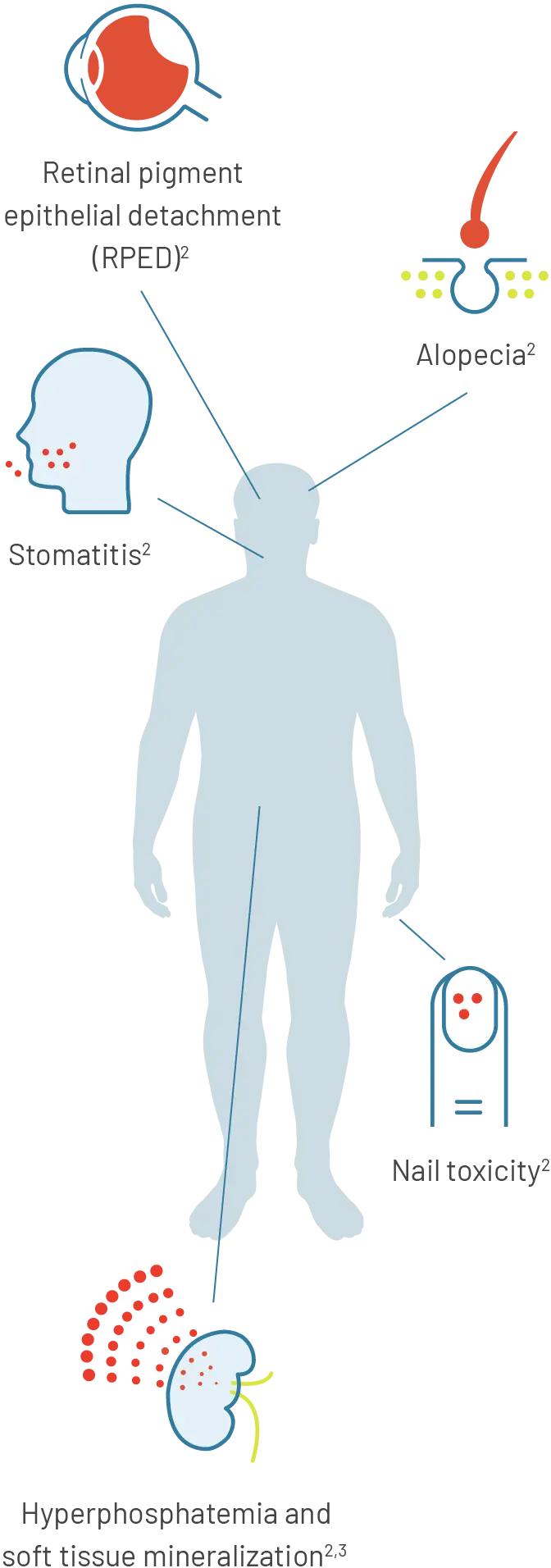
Select adverse reactions with PEMAZYRE, an inhibitor of FGFR1, 2, and 31
For more information on adverse reactions with PEMAZYRE, please visit the Safety page.
Retinal pigment epithelial detachment (RPED)
Monitoring
Advise patients to inform you of any vision changes while taking PEMAZYRE.1
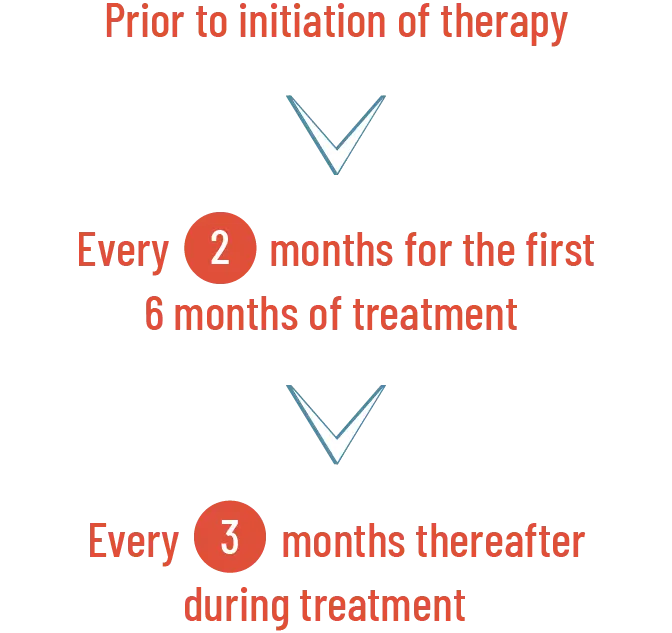
Perform a comprehensive ophthalmological examination, including optical coherence tomography (OCT), prior to initiation of PEMAZYRE, every 2 months for the first 6 months of treatment, and every 3 months thereafter during treatment.1
OCT is a non-invasive imaging test that uses light waves to map and measure the thickness of distinctive layers of the retina.4

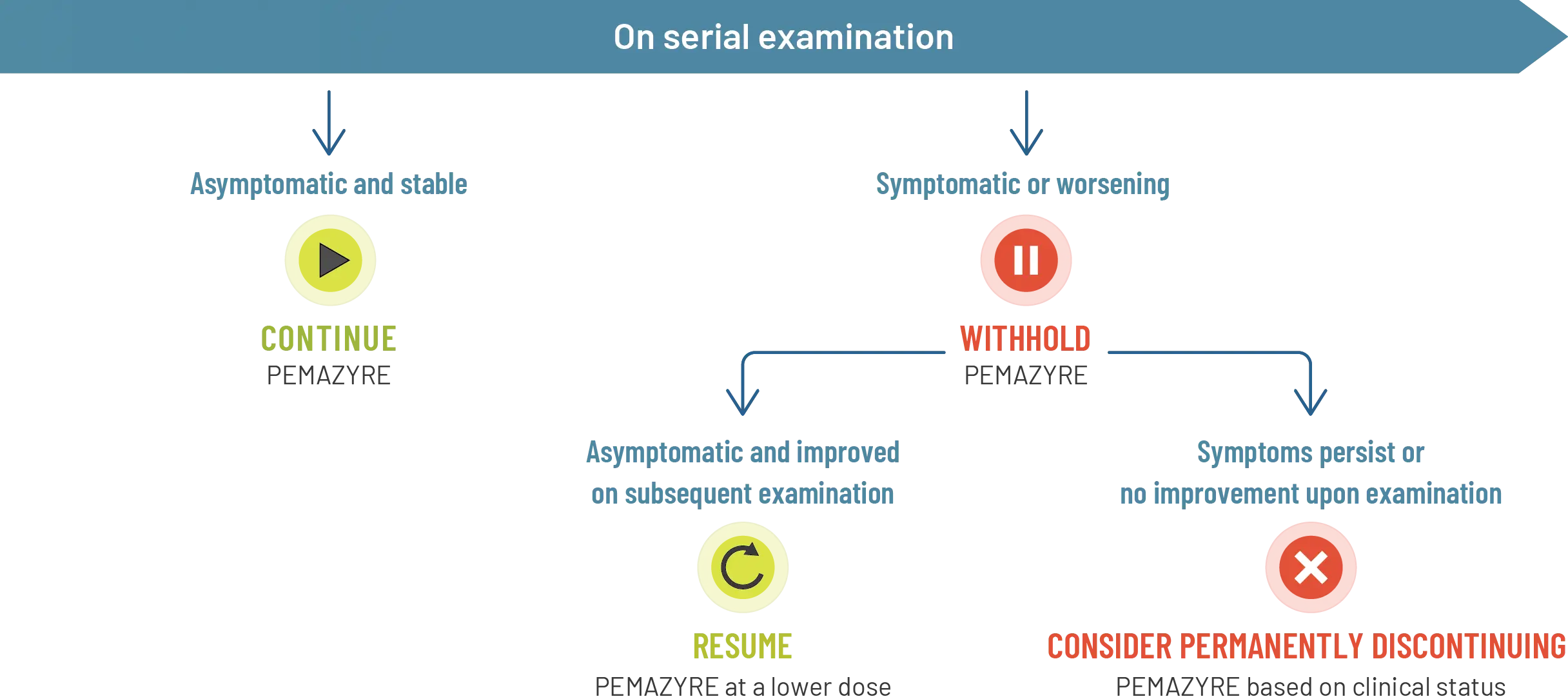
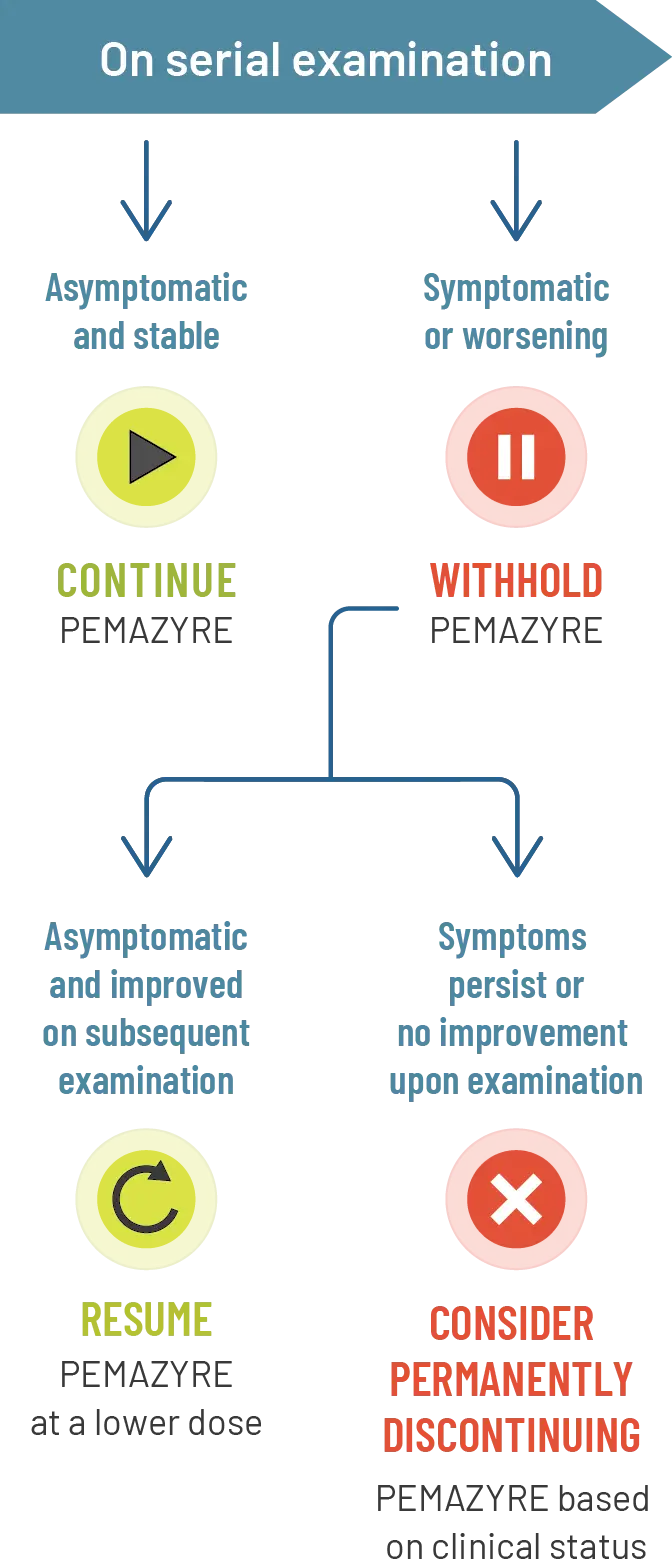
Management
- For onset of visual symptoms, refer patient for ophthalmologic evaluation urgently, with follow-up every 3 weeks until resolution or discontinuation of PEMAZYRE1
- Modify the dose or permanently discontinue PEMAZYRE as recommended1

Management of RPED in clinical trials
Among 635 patients who received a starting dose of PEMAZYRE 13.5 mg across clinical trials, RPED occurred in 11% of patients, including Grade 3-4 RPED in 1.3%.1
The median time to first onset of RPED was 56 days
Dose modifications:
- RPED resolved or improved to Grade 1 levels in 76% of patients who required dosage modification for RPED
- 1.3% of patients required dose reduction for RPED
- RPED led to dose interruption of PEMAZYRE in 3.1% of patients
- 0.2% of patients permanently discontinued treatment due to RPED
Clinical trials of PEMAZYRE did not conduct routine monitoring, including OCT, to detect asymptomatic RPED; therefore, the incidence of asymptomatic RPED with PEMAZYRE is unknown.1
Scientific Background
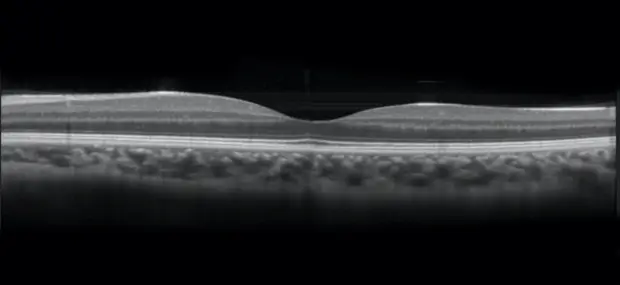
OCT image of normal retina. Reprinted with permission.5
The FGF/FGFR pathway plays an essential role in the retinal epithelium.
Fibroblast growth factor (FGF) is a neurotrophic factor found in the retinal pigment epithelium (RPE)
FGF promotes growth in immature RPE cells and helps prevent apoptosis of mature cells
FGFR-mitogen-activated protein kinase (MAPK) signaling helps protect the RPE from injury
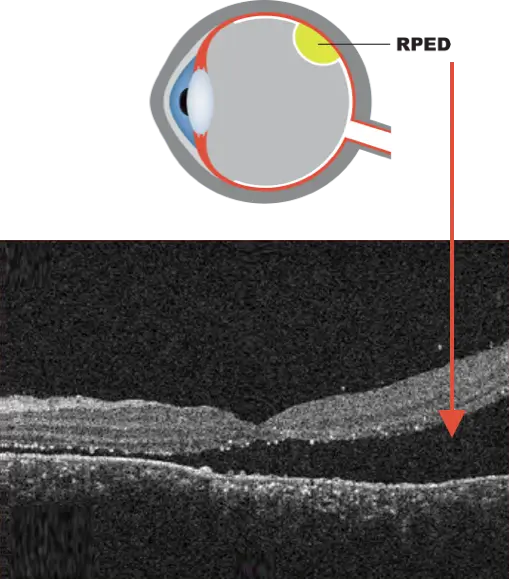
OCT image of exudative retinal detachment.7 Adapted from Simunovic MP, et al. BMC Ophthalmol. 2020;20(1):349.
RPED is characterized by the accumulation of fluid under the retina.6
RPED does not represent an actual, physical tear or separation of the retina5
Treatment of RPED is conservative; it often resolves within days without requiring treatment5
PEMAZYRE is an FGFR1, 2, and 3 inhibitor and therefore can cause RPED; this may cause symptoms such as blurred vision, visual floaters, or photopsia.1,2,5
Hyperphosphatemia and soft tissue mineralization
Monitoring
Monitor for hyperphosphatemia. Inform patients that they may experience an increase in phosphate levels and of the need to monitor serum phosphate levels. Advise patients to immediately inform their healthcare provider of any symptoms related to acute change in phosphate levels, such as muscle cramps, numbness, or tingling around the mouth.1
Management

Management of hyperphosphatemia in clinical trials
Among 635 patients who received a starting dose of PEMAZYRE 13.5 mg across clinical trials1:
Hyperphosphatemia was reported in 93% of patients based on laboratory values above the upper limit of normal
The median time to onset of hyperphosphatemia was 8 days (range, 1-169)
Phosphate-lowering therapy was required in 33% of patients receiving PEMAZYRE
Scientific Background
Increase in phosphate levels is a related effect of FGFR inhibition8-10
FGF23, an FGFR ligand, is involved in phosphate homeostasis by reducing uptake of phosphate by the kidney.
FGFR inhibition may lead to blockade of FGF23 signaling and in turn cause hyperphosphatemia.
Hyperphosphatemia is often asymptomatic11
Hyperphosphatemia can be associated with soft tissue and organ calcification3
Dermatologic/mucosal adverse reactions12
Management
Consider counseling and education on the potential for nail changes before initiation of treatment.12
Preventative strategies may include avoidance of12:
- Prolonged contact with water
- Repeated trauma
- Friction
- Pressure on the nails and nail beds
Patients may be advised to12:
- Limit the use of nail polish removers or hardeners
- Avoid biting nails or cutting nails too short
- Use topical emollients
- Wear loose-fitting socks and footwear
Preventative correction of nail curvature may be considered.12
Consider counseling and education on the potential for stomatitis before initiation of treatment.12
Preventative strategies may include12:
- Dental work to address tooth and gum disease before start of treatment
- Education regarding the importance of thorough and frequent cleaning of the oral cavity
Patients may be advised to12:
- Avoid salty, spicy, or citrus-based foods
- Avoid hot beverages
Potential management approaches may include use of13:
- Coating agents, such as bismuth salicylate, sucralfate, or other antacids
- Water-soluble mouth/lip lubricants
- “Magic mouthwash” (may include antifungals, antibacterials, steroids, and/or local anesthetics)
- Topical or oral analgesics
- Topical anesthetics
Preventative measures normally considered for patients undergoing traditional chemotherapy (eg, scalp compression, scalp cooling, medications) may not be applicable.12
Management approaches to consider may include12:
- Prophylactic or reactive topical medications for the scalp to encourage hair regrowth
- High-potency topical corticosteroids
- Camouflaging methods that create the appearance of naturally fuller hair
Attention should be focused on early identification and management.12
Scientific Background
FGFR inhibition and dermatologic events12
Nail toxicity, stomatitis, and alopecia have been observed with FGFR inhibition.
The pathophysiological mechanisms of these events are not fully understood.
Several possible mechanisms have been proposed, including:
- Inhibition of FGFR in keratinocytes, inducing dysregulation of hair-follicle homeostasis and epidermal proliferation
- Inhibition of hormonal FGF signaling by FGF19, FGF21, and FGF23
For additional information about adverse reactions and dose modifications, please see the Full Prescribing Information for PEMAZYRE.
Indications and Usage
PEMAZYRE® is indicated for the treatment of adults with relapsed or refractory myeloid/lymphoid neoplasms (MLNs) with fibroblast growth factor receptor 1 (FGFR1) rearrangement.
Important Safety Information
Ocular Toxicity
Retinal Pigment Epithelial Detachment (RPED): PEMAZYRE can cause RPED, which may cause symptoms such as blurred vision, visual floaters, or photopsia. Clinical trials of PEMAZYRE did not conduct routine monitoring including optical coherence tomography (OCT) to detect asymptomatic RPED; therefore, the incidence of asymptomatic RPED with PEMAZYRE is unknown.
Among 635 patients who received a starting dose of PEMAZYRE 13.5 mg across clinical trials, RPED occurred in 11% of patients, including Grade 3-4 RPED in 1.3%. The median time to first onset of RPED was 56 days. RPED led to dose interruption of PEMAZYRE in 3.1% of patients, and dose reduction and permanent discontinuation in 1.3% and in 0.2% of patients, respectively. RPED resolved or improved to Grade 1 levels in 76% of patients who required dosage modification of PEMAZYRE for RPED.
Perform a comprehensive ophthalmological examination including OCT prior to initiation of PEMAZYRE and every 2 months for the first 6 months and every 3 months thereafter during treatment. For onset of visual symptoms, refer patients for ophthalmologic evaluation urgently, with follow-up every 3 weeks until resolution or discontinuation of PEMAZYRE. Modify the dose or permanently discontinue PEMAZYRE as recommended in the prescribing information for PEMAZYRE.
Dry Eye: Among 635 patients who received a starting dose of PEMAZYRE 13.5 mg across clinical trials, dry eye occurred in 31% of patients, including Grade 3-4 in 1.6% of patients. Treat patients with ocular demulcents as needed.
Hyperphosphatemia and Soft Tissue Mineralization
PEMAZYRE can cause hyperphosphatemia leading to soft tissue mineralization, cutaneous calcification, calcinosis, and non-uremic calciphylaxis. Increases in phosphate levels are a pharmacodynamic effect of PEMAZYRE. Among 635 patients who received a starting dose of PEMAZYRE 13.5 mg across clinical trials, hyperphosphatemia was reported in 93% of patients based on laboratory values above the upper limit of normal. The median time to onset of hyperphosphatemia was 8 days (range 1-169). Phosphate lowering therapy was required in 33% of patients receiving PEMAZYRE.
Monitor for hyperphosphatemia and initiate a low phosphate diet when serum phosphate level is >5.5 mg/dL. For serum phosphate levels >7 mg/dL, initiate phosphate lowering therapy and withhold, reduce the dose, or permanently discontinue PEMAZYRE based on duration and severity of hyperphosphatemia as recommended in the prescribing information.
Embryo-Fetal Toxicity
Based on findings in an animal study and its mechanism of action, PEMAZYRE can cause fetal harm when administered to a pregnant woman. Oral administration of pemigatinib to pregnant rats during the period of organogenesis caused fetal malformations, fetal growth retardation, and embryo-fetal death at maternal exposures lower than the human exposure based on area under the curve (AUC) at the clinical dose of 13.5 mg.
Advise pregnant women of the potential risk to the fetus. Advise female patients of reproductive potential to use effective contraception during treatment with PEMAZYRE and for 1 week after the last dose. Advise males with female partners of reproductive potential to use effective contraception during treatment with PEMAZYRE and for 1 week after the last dose.
Adverse Reactions: Myeloid/Lymphoid Neoplasms with FGFR1 Rearrangement
Serious adverse reactions occurred in 53% of patients receiving PEMAZYRE at all dosages (n=34). Serious adverse reactions in > 5% of patients included acute kidney injury. Fatal adverse reactions occurred in 9% of patients who received PEMAZYRE, including acute kidney injury, multiple organ dysfunction syndrome, and malignant neoplasm progression, occurring in one patient each.
Permanent discontinuation due to an adverse reaction occurred in 12% of patients who received PEMAZYRE at all dosages. Adverse reactions requiring permanent discontinuation included cardiac failure, multiple organ dysfunction syndrome, blood alkaline phosphatase increase, and calciphylaxis. In patients who started treatment on the recommended dosage (n = 20), adverse reactions requiring dosage interruption of PEMAZYRE occurred in 80% of patients. Adverse reactions which required dosage interruption in > 2 patients treated at the recommended dosage included nail toxicities (20%) and hyperphosphatemia (15%).
Dose reductions of PEMAZYRE due to an adverse reaction occurred in 80% of patients who started treatment on the recommended dosage. Adverse reactions requiring dose reductions occurring in > 2 patients were nail toxicities (20%), hyperphosphatemia (20%), and alopecia (15%).
Clinically relevant adverse reactions occurring in ≤10% of patients included fractures (2.1%). In all patients treated with pemigatinib, 0.5% experienced pathologic fractures (which included patients with and without cholangiocarcinoma [N = 635]). Soft tissue mineralization, including cutaneous calcification, calcinosis, and non-uremic calciphylaxis associated with hyperphosphatemia were observed with PEMAZYRE treatment.
Within the first 21-day cycle of PEMAZYRE dosing, serum creatinine increased (mean increase of 0.2 mg/dL) and reached steady state by Day 8, and then decreased during the 7 days off therapy. Consider alternative markers of renal function if persistent elevations in serum creatinine are observed.
The most common (≥ 20%) adverse reactions were hyperphosphatemia (74%), nail toxicity (62%), alopecia (59%), stomatitis (53%), diarrhea (50%), dry eye (50%), fatigue (44%), rash (35%), abdominal pain (35%), anemia (35%), constipation (32%), dry mouth (32%), epistaxis (29%), retinal pigment epithelial detachment (26%), extremity pain (26%), decreased appetite (24%), dry skin (24%), dyspepsia (24%), back pain (24%), nausea (21%), blurred vision (21%), peripheral edema (21%), and dizziness (21%).
Drug Interactions
Avoid concomitant use of strong and moderate CYP3A inhibitors with PEMAZYRE. Reduce the dose of PEMAZYRE if concomitant use with a strong or moderate CYP3A inhibitor cannot be avoided. Avoid concomitant use of strong and moderate CYP3A inducers with PEMAZYRE.
Special Populations
Advise lactating women not to breastfeed during treatment with PEMAZYRE and for 1 week after the last dose.
Reduce the recommended dose of PEMAZYRE for patients with severe renal impairment as described in the prescribing information.
Reduce the recommended dose of PEMAZYRE for patients with severe hepatic impairment as described in the prescribing information.
Please see Full Prescribing Information for PEMAZYRE.
Indications and Usage
PEMAZYRE® is indicated for the treatment of adults with relapsed or refractory myeloid/lymphoid neoplasms (MLNs) with fibroblast growth factor receptor 1 (FGFR1) rearrangement.
Important Safety Information
Ocular Toxicity
Retinal Pigment Epithelial Detachment (RPED): PEMAZYRE can cause RPED, which may cause symptoms such as blurred vision, visual floaters, or photopsia. Clinical trials of PEMAZYRE did not conduct routine monitoring including optical coherence tomography (OCT) to detect asymptomatic RPED; therefore, the incidence of asymptomatic RPED with PEMAZYRE is unknown.
Among 635 patients who received a starting dose of PEMAZYRE 13.5 mg across clinical trials, RPED occurred in 11% of patients, including Grade 3-4 RPED in 1.3%. The median time to first onset of RPED was 56 days. RPED led to dose interruption of PEMAZYRE in 3.1% of patients, and dose reduction and permanent discontinuation in 1.3% and in 0.2% of patients, respectively. RPED resolved or improved to Grade 1 levels in 76% of patients who required dosage modification of PEMAZYRE for RPED.
Perform a comprehensive ophthalmological examination including OCT prior to initiation of PEMAZYRE and every 2 months for the first 6 months and every 3 months thereafter during treatment. For onset of visual symptoms, refer patients for ophthalmologic evaluation urgently, with follow-up every 3 weeks until resolution or discontinuation of PEMAZYRE. Modify the dose or permanently discontinue PEMAZYRE as recommended in the prescribing information for PEMAZYRE.
Dry Eye: Among 635 patients who received a starting dose of PEMAZYRE 13.5 mg across clinical trials, dry eye occurred in 31% of patients, including Grade 3-4 in 1.6% of patients. Treat patients with ocular demulcents as needed.
Hyperphosphatemia and Soft Tissue Mineralization
PEMAZYRE can cause hyperphosphatemia leading to soft tissue mineralization, cutaneous calcification, calcinosis, and non-uremic calciphylaxis. Increases in phosphate levels are a pharmacodynamic effect of PEMAZYRE. Among 635 patients who received a starting dose of PEMAZYRE 13.5 mg across clinical trials, hyperphosphatemia was reported in 93% of patients based on laboratory values above the upper limit of normal. The median time to onset of hyperphosphatemia was 8 days (range 1-169). Phosphate lowering therapy was required in 33% of patients receiving PEMAZYRE.
Monitor for hyperphosphatemia and initiate a low phosphate diet when serum phosphate level is >5.5 mg/dL. For serum phosphate levels >7 mg/dL, initiate phosphate lowering therapy and withhold, reduce the dose, or permanently discontinue PEMAZYRE based on duration and severity of hyperphosphatemia as recommended in the prescribing information.
Embryo-Fetal Toxicity
Based on findings in an animal study and its mechanism of action, PEMAZYRE can cause fetal harm when administered to a pregnant woman. Oral administration of pemigatinib to pregnant rats during the period of organogenesis caused fetal malformations, fetal growth retardation, and embryo-fetal death at maternal exposures lower than the human exposure based on area under the curve (AUC) at the clinical dose of 13.5 mg.
Advise pregnant women of the potential risk to the fetus. Advise female patients of reproductive potential to use effective contraception during treatment with PEMAZYRE and for 1 week after the last dose. Advise males with female partners of reproductive potential to use effective contraception during treatment with PEMAZYRE and for 1 week after the last dose.
Adverse Reactions: Myeloid/Lymphoid Neoplasms with FGFR1 Rearrangement
Serious adverse reactions occurred in 53% of patients receiving PEMAZYRE at all dosages (n=34). Serious adverse reactions in > 5% of patients included acute kidney injury. Fatal adverse reactions occurred in 9% of patients who received PEMAZYRE, including acute kidney injury, multiple organ dysfunction syndrome, and malignant neoplasm progression, occurring in one patient each.
Permanent discontinuation due to an adverse reaction occurred in 12% of patients who received PEMAZYRE at all dosages. Adverse reactions requiring permanent discontinuation included cardiac failure, multiple organ dysfunction syndrome, blood alkaline phosphatase increase, and calciphylaxis. In patients who started treatment on the recommended dosage (n = 20), adverse reactions requiring dosage interruption of PEMAZYRE occurred in 80% of patients. Adverse reactions which required dosage interruption in > 2 patients treated at the recommended dosage included nail toxicities (20%) and hyperphosphatemia (15%).
Dose reductions of PEMAZYRE due to an adverse reaction occurred in 80% of patients who started treatment on the recommended dosage. Adverse reactions requiring dose reductions occurring in > 2 patients were nail toxicities (20%), hyperphosphatemia (20%), and alopecia (15%).
Clinically relevant adverse reactions occurring in ≤10% of patients included fractures (2.1%). In all patients treated with pemigatinib, 0.5% experienced pathologic fractures (which included patients with and without cholangiocarcinoma [N = 635]). Soft tissue mineralization, including cutaneous calcification, calcinosis, and non-uremic calciphylaxis associated with hyperphosphatemia were observed with PEMAZYRE treatment.
Within the first 21-day cycle of PEMAZYRE dosing, serum creatinine increased (mean increase of 0.2 mg/dL) and reached steady state by Day 8, and then decreased during the 7 days off therapy. Consider alternative markers of renal function if persistent elevations in serum creatinine are observed.
The most common (≥ 20%) adverse reactions were hyperphosphatemia (74%), nail toxicity (62%), alopecia (59%), stomatitis (53%), diarrhea (50%), dry eye (50%), fatigue (44%), rash (35%), abdominal pain (35%), anemia (35%), constipation (32%), dry mouth (32%), epistaxis (29%), retinal pigment epithelial detachment (26%), extremity pain (26%), decreased appetite (24%), dry skin (24%), dyspepsia (24%), back pain (24%), nausea (21%), blurred vision (21%), peripheral edema (21%), and dizziness (21%).
Drug Interactions
Avoid concomitant use of strong and moderate CYP3A inhibitors with PEMAZYRE. Reduce the dose of PEMAZYRE if concomitant use with a strong or moderate CYP3A inhibitor cannot be avoided. Avoid concomitant use of strong and moderate CYP3A inducers with PEMAZYRE.
Special Populations
Advise lactating women not to breastfeed during treatment with PEMAZYRE and for 1 week after the last dose.
Reduce the recommended dose of PEMAZYRE for patients with severe renal impairment as described in the prescribing information.
Reduce the recommended dose of PEMAZYRE for patients with severe hepatic impairment as described in the prescribing information.
Please see Full Prescribing Information for PEMAZYRE.